Chest Drainage
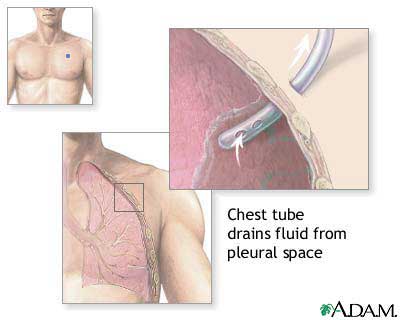
The chest drain is required when a patient has an
air leak (pneumothorax), a collection of fluid (pleural effusion) or a
collection of pus (empyema) in the pleural space. Any of these can cause
problems with breathing and can stop the lungs from working properly. The chest
drain will allow the fluid or air to leave the body and allow the lungs to
re-expand.
A chest drain is a narrow tube that is inserted and
sits in the space between the lung and the chest wall. This space is lined on
both sides by a membrane called the pleura and is known as the pleural cavity or
pleural space.
A chest drain is inserted when air, fluid or pus has
collected in the pleural space.
The external end of the chest drain tube is attached
to a bottle containing water which acts as a seal to prevent air from leaking
back into the pleural space.
Working of a Chest Drain:
Once a chest drain is inserted it is connected to a bottle which contains
water. The fluid or air then travels down the tube, into the bottle with the
water acting as a seal preventing air or fluid coming back up the tube into the
chest.
Insertion:
The procedure is performed using an aseptic technique to minimize the risk
of infection. The skin of the patient has to be cleaned with an alcohol cleaner
to kill any bacteria and a local anesthetic is then injected to numb the area
where the tube is to be inserted, this can ‘sting’ temporarily but resolves
quickly. A small cut is then made in the anaesthetized area and the doctor
gently opens up a path for the chest drain. It is normal to feel a sensation of
pressure and tugging as the drain is gently eased into the chest.
The chest drain is held in place with stitches and the exit site is covered with
gauze and a waterproof dressing. The end of the tubing is connected to a
drainage bottle which acts as the underwater seal and collection chamber. The
chest drain will be monitored regularly.
Suction:
Occasionally a lung needs some help to re-expand. If so the drainage bottle
can be connected to a suction unit on the wall using a long piece of tubing. The
gentle suction provided will help the lung re-expand.
Does and Don’ts of Chest Drains:
As the fluid or air around the lung drains the patient should be able to
move more easily.
There are a few simple rules that can follow to minimize any problems:
-
Carry the drainage bottle below the level of
waist. If it is lifted above to the waist level fluid from the bottle may flow
back into the pleural space
-
If the drainage is on suction to encourage lung
re-expansion it will be necessary to remain close to the bed as the suction
tube will limit the movement of the patient
-
If disconnection occurs reconnect and ask patient
to cough
-
If persistent air leak consider low pressure
suction
-
Whilst in bed keep the drainage bottle on the
floor
-
Do not pull on the chest drain or tangle
-
Do not swing the bottle by the tube
-
Observe for post-expansion pulmonary oedema
Removal:
The chest drain will stay in between one
day to many days depending on how well the patient respond to the treatment
during which several chest x-rays have been taken.
Removing the drain is a simple procedure. Once all the dressings are removed the
drain is gently pulled out. The doctor or nurse may ask the patient for
breathing in a particular way while the drain is removed. This can feel a little
uncomfortable but only lasts a few seconds.
After drain removal procedure is over, a stitch is often left where the drain
has been which will be removed after five to seven days.
Risks:
In most cases the insertion of a chest drain is a routine and safe procedure
and most people find breathing is much easier once the chest drain is in place.
However, like all medical procedures, chest drains can cause some problems.
Following are The Common Features of a Typical Chest Drainage Catheter:
-
Chest Drainage Catheter is used for post operative
drainage after cardio thoracic surgery.
-
Manufactured from non toxic, medical grade PVC
compound.
-
Smooth and round open distal end.
-
It is provided with large smooth eyes for maximum
drainage.
-
It is marked at every 2 cm from the last eye to
ascertain the depth of placement.
-
Proximal end of the catheter is fitted with Taper
tongue connecter to provide better forceps grip and smooth penetration
-
Available in right angle.
-
Sterile, individually packed in peelable pouch
pack
http://www.kendall-ltp.com/Kendall-LTP/pageBuilder.aspx?contentID=
67322&webPageID=0&topicID=67317&breadcrumbs=810 5:0,67274:0,191129:0 |